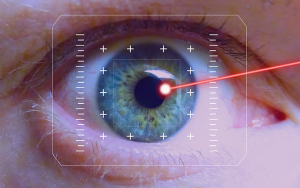
Advances in corneal topography and tomography are making it easier for doctors to see the whole picture. New imaging and screening technologies are helping ophthalmologists with ectasia risk screening, diagnosis and treatment of keratoconus, and post-LASIK ectasia. Placido disk technology was an earlier corneal imaging iteration and only examined the central anterior surface of the cornea, and generated anterior corneal shape-based indices.
When scanning slit-based technology was introduced, it was suddenly possible to image the posterior cornea. Since more information about the posterior surface elevation was available, doctors became more efficient at diagnosing conditions like keratoconus. Keratoconus, a condition where the cornea bulges out in a cone shape, affects 86 in 100,000 people and results in loss of vision. If ophthalmologists can diagnose this condition quickly enough, it's possible to stabilize the disease or even improve vision.
“Corneal topography and tomography allow precise measurement of anterior and posterior corneal curvatures and corneal thickness and enable the diagnosis, classification, and monitoring of progression of corneal diseases, but there can be more to the picture,” said Dr. Jhanji, professor ophthalmology, University of Pittsburgh. “Hopefully, these processes will be improved in the future through a combination of biomechanical factors, topographic indices, and surgery-induced risk-stratification.”
Innovations like Scheimpflug camera-based devices can image the central anterior, posterior cornea, and peripheral cornea in a new way. When paired with software systems, it can generate comprehensive diagnostic indices for identifying subclinical and frank keratoconus. When there is an abnormal topography present, there is a significant risk factor for post-LASIK ectasia. Consequently, it’s one of the most frequent indicators for topography/tomography in anterior segment practice when screening for ectasia risk.
Red flags for poor surgical candidates include image-based ID of irregularities such as asymmetric bowtie, skewed radial axis, or inferior/paraxial steepening or thinning. Also, different instruments can output calculated scores such as BCV index, Sirius; BAD-D, Pentacam; KISA%, Orbscan. “The reliability of these scores depends on the reliability of the individual factors that are used to calculate them,” said Jhanji. “However, interchange between devices can lead to extrapolation errors. For that reason, it is preferable to do serial follow-up using the same device.”
The process of Lasik involves the removal of cornea tissue and the reformation of the corneal wall. It's a helpful procedure that can treat nearsightedness, farsightedness, and astigmatism – but it also thins the cornea. Jhanji added that the risk of post-LASIK ectasia could also be affected by surgical and postsurgical influences that can't be explained by corneal topography/tomography.
For example, factors like corneal biomechanics, flap thickness variation, ablation volume, and decentration won't be captured by imaging technology. Jhanji argues that while serial imaging can reveal changes in individual factors or calculated indices can be understood as providing clear signs of ectasia development and progression – it's important to remember other variables require consideration before decisions about patient care are made.
In summary, software and hardware advances are changing the way corneal imaging is utilized, but the technology cannot account for all eventualities. "In all cases, clinical correlation is important," Jhanji said. “What looks like keratoconus on a topographic map may be a change caused by other corneal pathology.”